Pediatric Advance Life Support: SVT Part 1
"Too Fast" rhythms
· Sinus tachycardia
· Supraventricular tachycardia
· Ventricular tachycardia (with pulse)
· Wide complex tachycardia
Note: Just before the onset of pediatric cardiopulmonary failure, children may exhibit tachypnea and tachycardia, compensatory mechanisms that attempt to increase cardiac output and decrease acidosis. In most cases, blood pressure remains normal until cardiopulmonary failure is imminent. As oxygen demand increases and the child tires, compensatory mechanisms fail. The heart and respiratory rate decrease and blood pressure drops, signifying the onset of cardiopulmonary failure. Outcome is best if the child’s condition is recognized and treated aggressively before this point.
Treatment Approach
· Need for treatment is based upon the patient’s clinical condition
· Ask the question: “Is the patient stable or unstable?”
· Precise identification of the initial rhythm is not required for initial treatment
Signs of Instability
· Shock with hypotension
· Altered mental status
· Sudden collapse
· Cold, clammy skin
· Delayed capillary refill
· Absent or weak pulses
Note: A dysrhythmia is considered unstable if the rhythm disturbance adversely affects cardiac output, as evidenced by the presence of decreased responsiveness, hypotension, or respiratory failure. In older children and adolescents, chest pain due to ischemia may also be present.
 |
| Sinus tachycardia |
Sinus Tachycardia
· Nonspecific clinical sign
· Gradual onset
· Causes include hypoxemia, hypovolemia, hyperthermia, metabolic stress, toxins, pain, and anxiety
· Heart rate varies with activity
· P waves present/normal
· Rate < 180 child, < 220 infant
Note: In sinus tachycardia, the heart rate is usually less than 220 beats per minute in infants and 180 beats per minute in children. Beat-to-beat variability in rate is present, and the focused history frequently reveals an identifiable cause, such as fever, pain, anxiety, or dehydration. The heart rate should improve as the cause is treated
 |
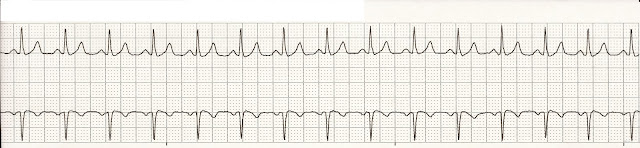
| Paroxysmal supraventricular tachycardia |
 |
| Supraventricular tachycardia |
SVT
· Can occur regularly or in paroxysms
· Abrupt onset or termination or both
· Reentry mechanism that involves accessory pathways or AV conduction system
· Produces heart rate >220 bpm in infants
· Produces heart rate >180 bpm in children
· Heart rate does not vary with activity
· P waves may be absent or abnormal
· History incompatible with sinus tachycardia
Note: This dysrhythmia is most often caused by an abnormal accessory conduction pathway that causes a reentrant electrical impulse. The reentrant impulse gets caught in a loop in the AV conduction system, and the heart is stimulated to contract at a faster rate.
In supraventricular tachycardia, the heart rate is usually faster than 220 beats per minute in infants or 180 beats per minute in children with no beat-to-beat variability in rate. The focused history is usually nonspecific.
Ventricular Tachycardia
· VT is uncommon in children
· Rate may vary from normal to > 200/min
· VT in children is usually associated with underlying heart disease
· Other causes include electrolyte disorders and drug toxicities
· Aberrant conduction present in < 10% of children, assume VT
 |
| Ventricular tachycardia |
Polymorphic VT (Torsades de pointes)
· QRS complexes vary in appearance
· The QRS complexes change in polarity and amplitude
· Ventricular rate ranges 150-250/min
· Associated with long QT interval, drug toxicities, congenital long QT syndrome
· Often occurs in “bursts” and spontaneously converts to another rhythm
 |
| Polymorphic VT |
Management of SVT
· Treat SVT with poor profusion with cardioversion
· May try brief trial of vagal maneuvers
· May give Adenosine if IV or IO access is immediately available



Comments
Post a Comment