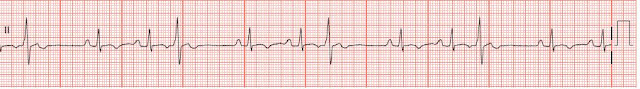
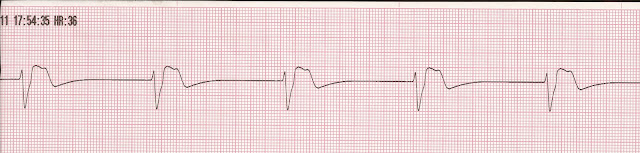
ACLS review: Acute Coronary Syndromes Part 1
Acute Coronary Syndromes Primary goals of therapy for patients with ACS · Reduce the amount of myocardial necrosis · Prevent major adverse cardiac events · Treat acute, life-threatening complications of ACS AMI Symptoms · Pain that is more intense than angina and that persists for longer periods of time (eg, longer than 15–20 minutes) · Chest discomfort, discomfort in other areas of the upper body, shortness of breath, sweating, nausea, vomiting, and dizziness · Atypical symptoms are more common in women, the elderly and diabetic patients. Initial Evaluation · Obtain vital signs and oxygen saturation · Obtain IV access · Obtain 12 lead EKG · Perform target history · Obtain serum cardiac enzymes, CBC chemistries, and coagulation studies · Portable CXR Note: Ideally within 10 minutes of ED arrival providers should obtain a targeted history while a monitor is attached to the