ACLS review: SVT part 6
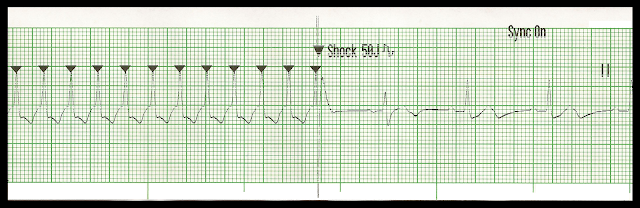
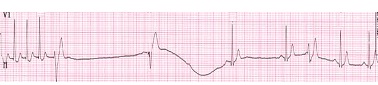
Synchronized cardioversion · Specific timed delivery of electrical shock to the heart · Treatment of choice for SVT, VT with a pulse and atrial flutter with evidence of poor profusion · Provide sedation and analgesia · Prepare to defibrillate immediately if cardioversion causes VF Note Synchronized cardioversion is shock delivery that is timed (synchronized) with the QRS complex. This synchronization avoids shock delivery during the relative refractory period of the cardiac cycle when a shock could produce VF. Indications · All tachycardias (rate >150 bpm) with serious signs and symptoms related to the tachycardia. These include unstable SVT, atrial flutter, atrial fibrillation and unstable VT · May give brief trial of medications based on specific arrhythmias. Note Cardioversion is less likely to be effective for treatment of junctional tachycardia or ectopic or multifocal atrial tach