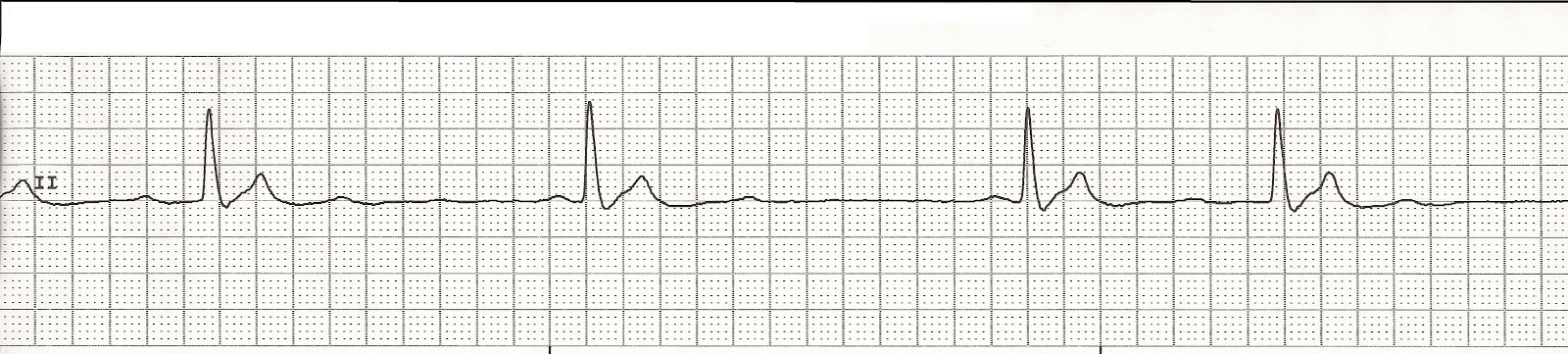
Code Blue: PEA

Near, far, wherever you are I believe that the heart does go on… 09:53 Placed on monitor Initial rhythm 09:55 CPR Unsuccessful IV access attempt Unsuccessful IV access attempt CPR Rhythm 10:00 CPR Intubated 7.5 ET tube. Tube placement confirmed CPR Rhythm 10:02 Epinephrine 2mg via ET tube Successful IO placement in right tibia CPR in progress CPR Rhythm 10:05 Vasopressin 40 units IO CPR in progress CPR Rhythm Check 10:09 Epinephrine 1mg IO NS fluid bolus started CPR Rhythm 10:11 Sodium Bicarbonate IO CPR in progress Adequate ventilations CPR Rhythm Check 10:15 Epinephrine 1mg IO CPR in progress CPR Rhythm 10:19 Epinephrine 1mg IO CPR in progress CPR Rhythm Check 10:24 Epinephrine 1mg IO CPR in progress CPR Rhythm 10:27 Epinephrine 1mg IO Continued CPR Final rhythm 10:28 Code ended Once more you open the door And you're here