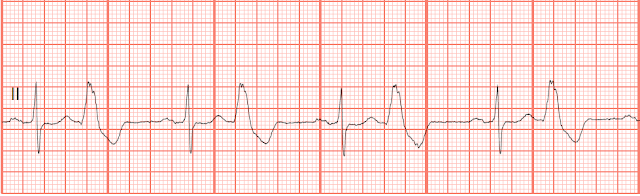
EKG Quiz 316

01. Identify the following rhythm: a. Sinus rhythm with unifocal PVCs b. Sinus tachycardia with unifocal PVC c. Sinus bradycardia with bigeminal PVCs d. Sinus rhythm with multifocal PVCs 02. Identify the following rhythm: a. Atrial flutter with a PVC b. Atrial fibrillation with a PVC c. Sinus rhythm with a PAC d. Sinus bradycardia with a PJC 03. Identify the following rhythm: a. Idioventricular rhythm with a salvo of PVCs b. Sinus bradycardia with nonsustained VT c. Ventricular pacing with a triplet of PVCs d. Junctional rhythm with consecutive PVCs 04. Identify the following rhythm: a. Sinus arrhythmia with PACs b. Sinus bradycardia with a couple of PACs c. Sinus rhythm with unifocal PVCs d. Sinus rhythm with some PJCs 05. Identify the following rhythm: a. Sinus bradycardia with unifocal PVCs b. Sinus bradycardia with bigeminal PACs c. Sinus bradycardia with trigeminal l PVCs d. Sinus bradycardia with multif