Megacode Pulseless VF/VT Part 2
6/25/12
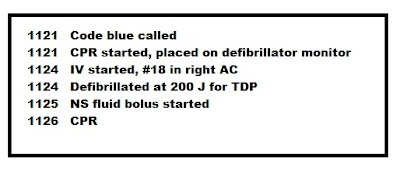
11:26. CPR is in progress and
ventilations remain adequate with good chest rise so intubation is deferred at
this time.
11. What is the first vasoconstrictor that is administered during a pulseless arrest?
12. After the initial defibrillation, what are the subsequent joule settings in the treatment of pulseless VT/VF?
a. Monophasic
b. Biphasic
13. Name three advantage of using an oropharyngeal airway (OPA) on an unconscious victim in cardiac arrest?
a.
b.
c.
12. After the initial defibrillation, what are the subsequent joule settings in the treatment of pulseless VT/VF?
a. Monophasic
b. Biphasic
13. Name three advantage of using an oropharyngeal airway (OPA) on an unconscious victim in cardiac arrest?
a.
b.
c.
14. What are some precautions that should be observed before applying the defibrillator pads to the patient?
a.
b.
c.
d.
e.
a.
b.
c.
d.
e.
15. During the treatment of pulseless VF/VT, how often can epinephrine be repeated?
6/25/12 11:28. Epinephrine has been given followed by a rhythm check. The patient remains in this refractory rhythm. A second defibrillation is given at 300J is given without a change in the rhythm. CPR is resumed. Ventilations remain adequate. The saline bolus is in progress.
16. What are some conditions that may predispose a patient to torsades de pointes?
a.
b.
c.
d.
17. What are the ECG characteristics of Torsades de pointes?
a.
b.
c.
d.
e.
f.
a.
b.
c.
d.
e.
f.
18. During CPR what is the difference in ventilation technique between an intubated patient and a non-intubated patient?
19. Name 5 medications that may be used in the treatment of pulseless VT?
a.
b.
c.
d.
e.
20. Name 4 facts related to the administration of Vasopressin
a.
b.
c.
d.
Answers to Questions
11. What is the first vasoconstrictor that is administered during a pulseless arrest?
Epinephrine 1mg IV push or Vasopressin 40 units IV push
12. After the initial defibrillation, what are the subsequent joule settings in the treatment of pulseless VT/VF?
a. 200 J or higher for biphasic defibrillators
b. 360 J for monophasic defibrillators
13. Name three advantage of using an oropharyngeal airway (OPA) on an unconscious victim in cardiac arrest?
a. The OPA holds the tongue in place and prevents it from occluding the airway
b.It may serve as a bite block in an intubated patient
c. It permits easy suctioning of the oropharynx.
14. What are some precautions that should be observed before applying the defibrillator pads to the patient?
a. Make sure the skin surface is dry
b. Avoid pacemakers and other devices
c. Avoid letting the pads touch
d. Remove medication patches
e. Remove excess chest hair if the pads do not adhere to the chest wall
15. During the treatment of pulseless VF/VT, how often can epinephrine be repeated?
Epinephrine 1mg IV every 3-5 minutes
16. What are some conditions that may predispose a patient to torsades de pointes?
a. Long QT syndrome
b. Hypomagnesaemia
c. Antiarrhythmic drug toxicity
d. Other drug toxicities: phenothiazines, tricyclic antidepressants, calcium channel blockers
17. During CPR what is the difference in ventilation technique between an intubated patient and a non-intubated patient?
With an intubated patient the rescuer gives continuous chest compressions without pauses for breaths while the person performing ventilations provides 8-10 breaths/minute.
18. What are the ECG characteristics of Torsades de pointes?
a. There are no P waves
b. There is no PR interval
c. The QRS complex appears wide, bizarre and changes from beat to beat
d. The amplitude of the QRS complex begins smaller and gets larger then begins to get smaller again.
e. The rate is usually over 150
f. The rhythm is irregular
19. Name 5 medications that may be used in the treatment of pulseless VT?
a. Epinephrine
b. Vasopressin
c. Amiodarone
d. Lidocaine
e. Magnesium
20. Name 4 facts related to the administration of Vasopressin
a. May give Vasopressin first or in place of 2nd dose of epinephrine
b. One time dose of 40 units only
c. May be given down the endotracheal tube
d. DO NOT double the dose for ET tube administration
19. Name 5 medications that may be used in the treatment of pulseless VT?
a.
b.
c.
d.
e.
20. Name 4 facts related to the administration of Vasopressin
a.
b.
c.
d.
Answers to Questions
11. What is the first vasoconstrictor that is administered during a pulseless arrest?
Epinephrine 1mg IV push or Vasopressin 40 units IV push
12. After the initial defibrillation, what are the subsequent joule settings in the treatment of pulseless VT/VF?
a. 200 J or higher for biphasic defibrillators
b. 360 J for monophasic defibrillators
13. Name three advantage of using an oropharyngeal airway (OPA) on an unconscious victim in cardiac arrest?
a. The OPA holds the tongue in place and prevents it from occluding the airway
b.It may serve as a bite block in an intubated patient
c. It permits easy suctioning of the oropharynx.
a. Make sure the skin surface is dry
b. Avoid pacemakers and other devices
c. Avoid letting the pads touch
d. Remove medication patches
e. Remove excess chest hair if the pads do not adhere to the chest wall
15. During the treatment of pulseless VF/VT, how often can epinephrine be repeated?
Epinephrine 1mg IV every 3-5 minutes
16. What are some conditions that may predispose a patient to torsades de pointes?
a. Long QT syndrome
b. Hypomagnesaemia
c. Antiarrhythmic drug toxicity
d. Other drug toxicities: phenothiazines, tricyclic antidepressants, calcium channel blockers
17. During CPR what is the difference in ventilation technique between an intubated patient and a non-intubated patient?
With an intubated patient the rescuer gives continuous chest compressions without pauses for breaths while the person performing ventilations provides 8-10 breaths/minute.
18. What are the ECG characteristics of Torsades de pointes?
a. There are no P waves
b. There is no PR interval
c. The QRS complex appears wide, bizarre and changes from beat to beat
d. The amplitude of the QRS complex begins smaller and gets larger then begins to get smaller again.
e. The rate is usually over 150
f. The rhythm is irregular
19. Name 5 medications that may be used in the treatment of pulseless VT?
a. Epinephrine
b. Vasopressin
c. Amiodarone
d. Lidocaine
e. Magnesium
20. Name 4 facts related to the administration of Vasopressin
a. May give Vasopressin first or in place of 2nd dose of epinephrine
b. One time dose of 40 units only
c. May be given down the endotracheal tube
d. DO NOT double the dose for ET tube administration





Comments
Post a Comment