ACLS Questions.
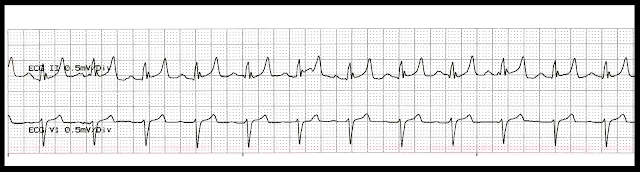
01. You respond to a Code Blue on the medical floor. The 56
year old patient with pancreatitis was found to be pulseless and apneic. When
you arrive to the room CPR is in progress and the patient is receiving positive
pressure ventilations. The ventilations
are adequate with good chest rise. The patient already had a # 18 saline lock
to the right AC. When the patient is
placed on the defibrillator monitor, the following rhythm is noted. What is the next appropriate intervention.
a. Administer a 1 mg epinephrine followed by a 10 cc
saline flush
b. Administer 300 mg of amiodarone followed by a 10 cc
saline flush
c. Begin transcutaneous pacing at 60 bpm
d. Give atropine 0.5 mg IV followed by a 10 cc saline
flush
02. A 75 year old is brought to the ER by his family with
complaints of shortness of breath, chest pain, and nausea and vomiting. The chest pain started two hours ago but
seemed to go away when he rested. But it
has since returned. A saline lock is established in his right AC and he is placed
on oxygen at 2 L/min. VS: 97.5-35-28. BP:
84/42. Oxygen Saturation: 91%. When
he is placed on the monitor the following rhythm is noted. What intervention is appropriate for the
patient at this time?
a. Administer nitroglycerin 0.4 mg SL up to three doses
b. Immediate transcutaneous pacing at 80 bpm
c. Epinephrine 1 mg IV or Vasopressin 40 units
d. Atropine 0.5 mg IV push followed by a 10 cc saline
flush
03. A 70 year old patient with a history of end stage renal
disease and is receiving hemodialysis is brought to the ER after falling and
with a suspected hip fracture. In route the patient became unresponsive and no spontaneous
respirations were noted. CPR was
initiated with positive pressure ventilations. The ventilations are noted to
adequate with good chest rise. The
patient was given Epinephrine 1 mg IV and Vasopressin 40 units in route. The
patient remains pulseless. When you
place the patient on the defibrillator/monitor, the following rhythm is
noted. What medications might be
considered for this rhythm?
a. Give Amiodarone 300 mg or Lidocaine 1 – 1.5 mg/kg IV
push
b. Give calcium gluconate, D50, and IV insulin 10 units
IV push
c. Vasopressin 40 units or epinephrine 1 mg IV push
d. Give Cardizem 10 mg or Lopressor 5 mg IV push
04. A 24 year old female who is currently taking some diet
pills comes to the ER complaining of shortness of breath, palpitations, and
weakness over the last 4 hours. She is
noted to be tachypneic and has some fine crackles in her bases. Her skin is cool and clammy. VS: 98.5-189-36. BP: 80/38. Sats: 90%. Oxygen at 2 L/min is started as
well as a saline lock with a fluid bolus.
When she is placed on the monitor, the following rhythm is noted. What is interventions would be appropriate
for the patient at this time?
a. Cardizem 0.35 mg/kg IV push, repeat at 0.25 mg/kg if
needed
b. Vagal maneuvers followed by Adenosine 12 mg rapid IV
push
c. Cardioversion at 50 joules
d. Defibrillation at 200 joules
05. A 56 year old construction worker is brought to the ER by
his foreman with complaints of severe chest pain that radiates to the left arm. Oxygen at 2 L/min is started and
nitroglycerin 0.4 mg is given X 3 for the chest pain with only moderate
relief. He suddenly becomes
unresponsive. No pulse is detected and a Code is called. CPR is in initiated.
The following rhythm is noted on the monitor. What intervention is appropriate
for this rhythm?
a. Vasopressin 40 units IV push followed by a 10 cc
saline flush
b. Epinephrine 1 mg IV push followed by a 10 cc saline
flush
c. Amiodarone 300 mg IV push followed by a 10 cc saline
flush
d. Defibrillate at 200 J
Answers
01. The answer is: a. Give epinephrine 1 mg IV push. During PEA a vasopressor should be given as soon as feasible with the primary goal of increasing myocardial and cerebral blood flow during CPR and achieving ROSC. B. Amiodarone is not recommended for pulseless electrical activity. C. Transcutaneous pacing is generally not effective in cardiac arrest, and no studies have observed a survival benefit from pacing in cardiac arrest. D. Available evidence suggests that the routine use of atropine during PEA or asystole is unlikely to have a therapeutic benefit.
02. The answer is: b. Immediate transcutaneous pacing. The patient has a complete heart block and is unstable with signs of poor perfusion. If the bradycardia is suspected to be the cause of acute altered mental status, ischemic chest discomfort, acute heart failure, hypotension, or other signs of shock, the patient should receive immediate treatment. Patients with a type II second-degree or third-degree AV block or in patients with third-degree AV block with a new wide-QRS complex are not likely to be responsive to reversal of cholinergic effects by atropine and are preferably treated with TCP or β-adrenergic support as temporizing measures while the patient is prepared for transvenous pacing. B. NTG is not recommended for a hypotensive patient. C. Epinephrine IV push is recommended for cardiac arrest, not in a patient with a pulse. D. Avoid relying on atropine in type II second-degree or third-degree AV block or in patients with third-degree AV block with a new wide-QRS complex where the location of block is likely to be in non-nodal tissue (such as in the bundle of His or more distal conduction system). These bradyarrhythmias are not likely to be responsive to reversal of cholinergic effects by atropine and are preferably treated with TCP or β-adrenergic support as temporizing measures while the patient is prepared for transvenous pacing
03. The answer is: b. Give calcium gluconate, D50, and IV insulin 10 units IV push. The ECG shows a sinus rhythm with tall, peaked, T waves. These are often seen with hyperkalemia. The patient has already received a round of vasoconstrictors so consideration of probable causes should be addressed. Treatment of severe hyperkalemia aims at protecting the heart from the effects of hyperkalemia by antagonizing the effect of potassium on excitable cell membranes, forcing potassium into cells to remove it promptly from the circulation, and removing potassium from the body. Calcium gluconate (10%): 15 to 30 mL IV over 2 to 5 minutes will decrease the excitability of the cardiac membrane. IV insulin will help drive the potassium into the cell. D50 will protect the patient against becoming hypoglycemic. A. Amiodarone is indicated for pulseless VF/VT, VT with a pulse, AF, and wide complex tachycardia. C. Vasopressin should not be repeated. Epinephrine can be repeated every 3 -5 minutes. Cardizem is indicated for treatment of tachyarrhythmias such as atrial fibrillation or atrial flutter.
04. The answer is: c. Cardioversion at 50 joules. The rhythm is a narrow complex tachycardia, SVT. The patient is unstable. If the patient demonstrates rate-related cardiovascular compromise with signs and symptoms such as acute altered mental status, ischemic chest discomfort, acute heart failure, hypotension, or other signs of shock suspected to be due to a tachyarrhythmia, proceed to immediate synchronized cardioversion. Cardioversion of SVTs generally requires less energy; an initial energy of 50 J to 100 J is often sufficient. A. Diltiazem would be recommend for refractory SVT or if the rhythm, is shown to be atrial fibrillation or atrial flutter. For diltiazem, give a dose of 15 mg to 20 mg (0.25 mg/kg) IV over 2 minutes; if needed, in 15 minutes give an additional IV dose of 20 mg to 25 mg (0.35 mg/kg). The maintenance infusion dose is 5 mg/hour to 15 mg/hour, titrated to heart rate. B. Vagal maneuvers and adenosine are the preferred initial therapeutic choices for the termination of stable PSVT. However, the initial dose of adenosine is 6 mg IV. The second dose is 12 mg. D. Defibrillation is recommended for pulseless VF/VT. If cardioversion is needed and it is impossible to synchronize a shock, use high-energy unsynchronized shocks (defibrillation doses).
05. The answer is: c. Defibrillate at 200 joules. The foundation of successful ACLS is high-quality CPR, and, for VF/pulseless VT, attempted defibrillation within minutes of collapse. For victims of witnessed VF arrest, early CPR and rapid defibrillation can significantly increase the chance for survival to hospital discharge. A and B. Vasoconstrictors are recommended if the VF/VT persist AFTER the first shock. C. Amiodarone is recommended for VF/VT that persists AFTER initial defibrillation attempts and the use of vasoconstrictors.








Comments
Post a Comment